
Mental Health Awareness Month: Meeting the Unprecedented Need
May is National Mental Health Awareness Month — a campaign to raise awareness about the realities faced by millions of Americans living with mental illness. Since our founding, we have worked to connect health and social care organizations to better support those in need.
As part of a person-centered approach, networks powered by Unite Us coordinate the provision of services for mental, physical, and social health needs, to provide wraparound care for every person. Because of the Unite Us Platform, an individual only has to tell their story once, which is particularly important if they are in crisis.
According to the World Health Organization, depression is the leading cause of disability worldwide. In the United States, the National Institute of Mental Health (NIMH) estimates that 57% of individuals with a mental health diagnosis go untreated. Since mental illness often co-occurs with other health issues and social needs, the cost can be personally devastating for individuals and their families, as well as for society. The COVID-19 pandemic has only exacerbated these struggles for millions of Americans.
The power of data to understand the problem and create solutions
The data generated by networks powered by Unite Us enables us to pull critical insights for our partners to understand not only the needs of their communities but the outcomes and impact of their coordinated efforts. Using the aggregate, de-identified data generated by these networks, we can answer many important questions in real-time. For example: what is client demand for services and how well are providers able to meet those needs? What needs are most likely to reoccur or appear together? Do we see differences in need, support provided, and outcomes across clients of different and intersecting identities?
The picture of mental health across our networks
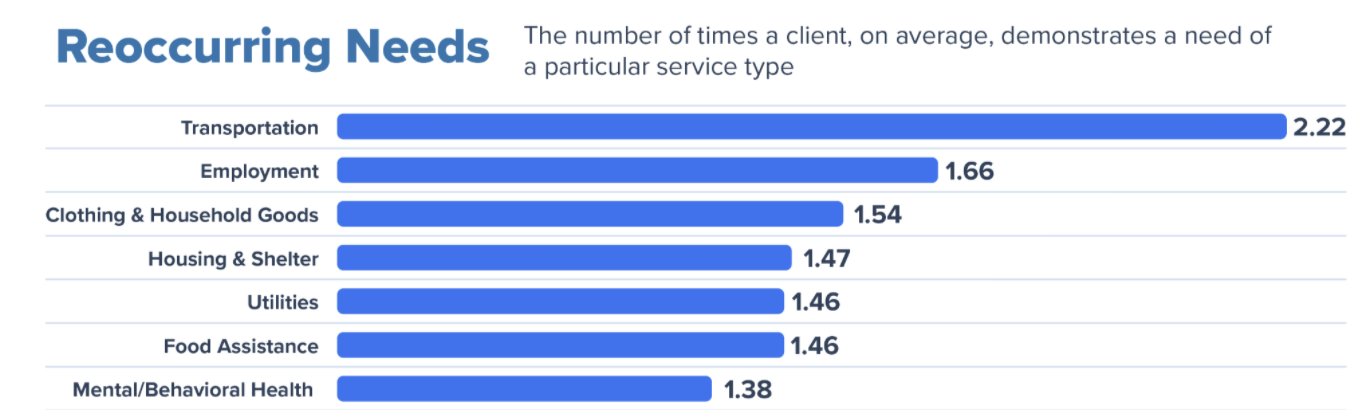
Mental/Behavioral Health is one of the most common (7th) reoccurring needs served through the Unite Us Platform, meaning individuals are commonly connected to Mental/Behavioral services more than once throughout their care journey. Having a coordinated network allows for a no wrong door approach to catch each of these times of need in a person’s care journey.
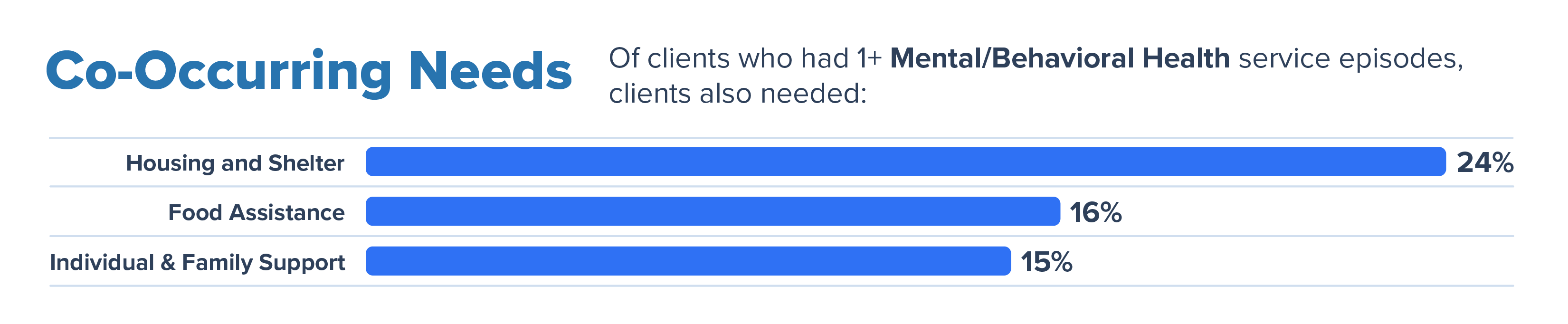
Similarly, a person facing one social care need, more often than not, is experiencing one or more co-occurring needs. Being able to address these co-occurring needs through your organization or easily referring to a network partner lessens the burden on the client. In our networks, we see these top 3 co-occurring needs for clients with a Mental/Behavioral Health need:
Unite Us’ approach to removing client burden and driving outcomes
At Unite Us, we know that barriers to mental health care and substance use services include access and affordability, lack of education about mental illness, and stigma. To address these challenges, we put the client at the center of their care, coordinating all mental, physical, and social health needs on a trauma-informed continuum of care.
Hear more about our approach in this new video featuring Alires Almon, Director of Innovation at the Mental Health Center of Denver, and our Virginia partners Dr. Patty Ferssizidis, Assistant Director, A Division for Advancing Prevention and Treatment, and Summer Jeirles, Manager, Behavioral Health Integration at Valley Health Behavioral Health Department.
“Instead of relying on the client to follow through on all this, when they are worried about if they’re going to eat that day, when they’re concerned about the weather and they have no shelter, trying to rely on them to do that is just too much. And so when we let them know ‘I’ve done the legwork for you and someone’s going to be reaching out to you,’ just the efficacy of that process makes it so much easier. This platform is so easy.“
– Summer Jeirles, Manager, Behavioral Health Integration at Valley Health Behavioral Health Department
Visibility and investment for the future
As the mental health crisis grows and gains visibility, state and federal governments are investing in solutions to address social determinants of health and increasing flexibility in spending to ensure outcomes. President Biden’s American Rescue Plan (ARP) presents enormous opportunities for improving community access to mental health and substance use services. The legislation allocates an additional $1.5 billion in both the Community Mental Health Services Block Grant (MHBG) and the Substance Abuse Prevention and Treatment Block Grant (SABG), which provide direct funding for community-based organizations, community mental health centers, substance use providers, and other related organizations. Beyond these block grants, the ARP also includes $80 million in community-based funding which the Substance Abuse and Mental Health Services Administration (SAMHSA) will distribute for behavioral health and substance use disorder services.
These investments are closely aligned with Unite Us’ mission to improve community health. We are committed to supporting our community partners as we build critical public health infrastructure together.
About Unite Us
Unite Us is the nation’s leading software company bringing sectors together to improve the health and well-being of communities. We drive the collaboration to predict, deliver, and pay for services that impact whole-person health. Through Unite Us’ national network and software, community-based organizations, government agencies, and healthcare organizations are all connected to better collaborate to meet the needs of the individuals in their communities.



